Project Aims
The D-CREDO project (2024-1-PL01-KA220-HED-000247790) equips health professions students and educators with the skills to effectively use digital health tools in clinical reasoning, cultivating a new generation of professionals who seamlessly integrate these tools into practice. Simultaneously, the project enhances educators’ confidence in embedding these tools into clinical reasoning curricula.
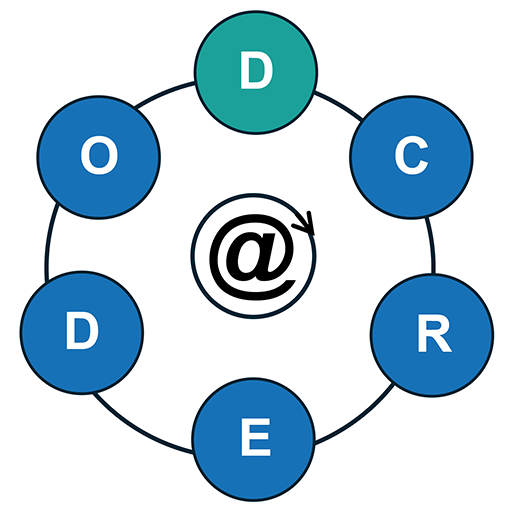
To accomplish these objectives, D-CREDO is organized into five work packages (WPs), each focused on a different aspect of the project presented in the figure.
The curriculum developed under D-CREDO follows the six-step curriculum design process outlined by David Kern: Problem Identification and General Needs Assessment, Targeted Needs Assessment, Goals and Objectives, Educational Strategies, Implementation, and Evaluation and Feedback, which is reflected in the division of project activities. The coordinator’s task is to ensure alignment across all work packages to maintain a consistent and high-quality curriculum. The project uses online collaborative tools and project management platforms to organize its activities, with regular biweekly virtual meetings and occasional in-person gatherings as part of the first work package (WP1: Project Management).
The project starts with a joint rapid review of the most recent and relevant literature. This review will help establish learning objectives and guide the development of a white paper outlining recommended learning strategies. The experiences gathered throughout the project contributes to the creation of policies and implementation guidelines for integrating the learning units into local curricula. Together, these activities within the work package will shape the overarching educational framework of D-CREDO (WP2: Educational Framework).
In collaboration with international partners and representatives from various health professions, D-CREDO develops new or enhances existing open-access learning content. This content integrates into the DID-ACT curriculum, either as extensions to current learning units or as new units. To improve knowledge transfer, we demonstrate the use of digital health tools in a case-based format through interactive patient scenarios, either by developing new virtual patients or expanding those from the iCoViP project. Feedback collected during this process informs the subsequent refinement of learning units (WP3: Educational Developments).
The project also deepens the initial needs analysis at partner institutions, developing and adapting tools to measure progress toward the set learning objectives. The learning units are piloted and evaluated from multiple perspectives across participating institutions, ensuring that project outcomes meet the expectations of the target audience (WP4: Evaluation and Quality).
Finally, through targeted dissemination efforts in social media, network of associated partners, web page, research publications, D-CREDO raises awareness of its findings and encourages the adoption of its educational resources within the broader health professions community. The final stages of the project focus on developing a sustainability strategy to ensure the project’s long-term impact (WP5: Dissemination and Sustainability).
D-CREDO Digital Health Tools
Through the process of need analysis we have decided on five classes of digital health tools we would like to focus on in the context of clinical reasoning education. These are AI in image analysis, LLM & big data, mHealth apps & wearables, EHR & CDSS and Telehealth.
1. AI in image analysis
How do we define it?
AI in image analysis refers to the application of artificial intelligence techniques, particularly machine learning (ML) and deep learning (DL), to interpret and analyze visual data from images. Deep learning models, including convolutional neural networks (CNNs), are commonly used to perform tasks such as recognizing patterns, detecting objects, segmenting specific regions of interest, classifying features, and making predictions or diagnoses based on image content. In healthcare, these AI tools are widely used in medical imaging to identify abnormalities, assist in diagnosis, and improve the accuracy of image-based decision-making. This technology plays a critical role in fields such as radiology, pathology, and dermatology, where image interpretation is essential for clinical care.
How is it relevant to clinical reasoning?
The integration of AI in image analysis presents both opportunities and challenges for clinical reasoning. On the one hand, AI tools can enable mass-scale screening, offering faster and more efficient diagnosis, particularly in resource-limited settings. On the other hand, issues such as bias against certain populations – especially people of color due to unrepresentative datasets – automation bias, and challenges with the transferability of AI models across different countries can significantly impact the reliability of these tools in clinical practice. These factors influence the reasoning process clinicians must undertake when incorporating AI-generated insights into their decision-making.
Moreover, reasoning around AI-assisted image processing tasks – such as segmentation or highlighting regions of interest – requires case-based knowledge, especially in specific medical fields like dermatology or radiology. Clinicians need to critically assess AI outputs and contextualize them within the broader diagnostic picture, balancing automation with human expertise to ensure accurate and equitable patient care.
2. LLM and big data
How do we define it?
Large Language Models (LLMs), such as GPT-4, Claude, or Gemini, are advanced AI systems designed to process and generate human-like text based on vast datasets. These models assist in various tasks within healthcare, including translating languages, summarizing information, explaining complex definitions, and searching for rare disease information. LLMs are increasingly used in areas like medical documentation and patient counseling by transforming data into valuable insights. However, their use comes with risks, such as data privacy concerns and the possibility of generating inaccurate information, often referred to as hallucinations.
Big data, on the other hand, refers to extremely large and complex datasets that are difficult to manage and analyze using traditional data processing tools. In healthcare, big data comes from diverse sources such as electronic health records, wearable devices, medical imaging, and even social media platforms. AI technologies, including LLMs, are often used to process and analyze this data, uncovering patterns or trends that can inform decision-making in clinical practice.
How is it relevant to clinical reasoning?
The integration of LLMs into clinical reasoning holds great potential but also presents challenges. Healthcare professionals can use these models to summarize complex medical knowledge, translate information, or help identify rare conditions. However, risks like unintentionally copying personal data into publicly accessible models or relying on AI-generated content that may not always be accurate demand careful attention.
Moreover, the use of big data analytics, particularly from sources like social media, raises concerns about privacy, digital professionalism, and the ethical use of information for lifestyle or health-related advice. These issues are critical in the context of clinical reasoning, where patient care decisions must be informed and safeguarded against potential AI-related risks.
3. mHealth apps and wearables
How do we define it?
mHealth (mobile health) apps and wearables refer to mobile applications and connected devices designed to monitor, collect, and transmit health-related data in real time. Wearables include devices like smartwatches, fitness bands, and even textiles with embedded sensors, which track various health metrics such as physical activity, heart rate, sleep patterns, and more. mHealth apps can cover a wide range of functions, from tracking mental health and medication adherence to providing telemedicine services or offering lifestyle and fitness guidance. These technologies enable users to manage their health and wellness more actively while providing healthcare professionals with valuable patient data outside traditional clinical settings.
How is it relevant to clinical reasoning?
The integration of mHealth apps and wearables into clinical reasoning significantly impacts person-centered care. Wearable devices allow for real-time data collection, which helps healthcare professionals monitor conditions like heart rate variability, glucose levels, or sleep quality continuously, leading to more informed and personalized clinical decisions. This real-time feedback can directly influence the clinical reasoning process by helping practitioners adjust treatment plans based on ongoing health data, improving patient outcomes.
For example, selecting the right mHealth app to address mental well-being requires careful consideration of outcomes, credibility, and patient compliance. Clinicians need to assess whether the app aligns with the patient’s needs and if its recommendations can be integrated into broader care plans.
Additionally, mHealth tools have proven useful for clinical reasoning in austere conditions, such as in war zones or remote locations. These tools offer a way to monitor and manage patients when traditional healthcare infrastructure is unavailable, providing critical support to both patients and healthcare providers in challenging environments.
4. EHR and CDSS
How do we define it?
Electronic Health Records (EHR) are digital versions of patients’ medical histories, containing key clinical information such as doctor’s notes, discharge summaries, lab results, medication lists, and imaging reports. EHR systems are designed to streamline the storage and sharing of patient data, ensuring healthcare providers have access to comprehensive information at the point of care. Clinical Decision Support Systems (CDSS), on the other hand, are software tools integrated within EHR systems or used separately to assist healthcare professionals in making clinical decisions. CDSS provides evidence-based recommendations, drug safety alerts, and diagnostic support by analyzing patient data and offering clinical insights to enhance decision-making.
How is it relevant to clinical reasoning?
EHR systems play a critical role in clinical reasoning by serving as the central repository of a patient’s medical data. Healthcare professionals use key elements like notes, discharge letters, and lab values to gather and synthesize information needed for diagnosis and treatment decisions. However, the way information is stored and presented can pose challenges. For instance, data distributed across many separate patient notes can lead to problems such as inconsistencies, copy/paste errors, and information overload. These issues can hinder the clinician’s ability to write accurate summary statements and increase the risk of errors in the clinical reasoning process.
CDSS are valuable tools for supporting clinical reasoning, but they come with their own set of challenges. While CDSS can enhance diagnostic accuracy and medication safety by offering alerts on value ranges or potential drug interactions, there is a risk of complacency and automation bias. Clinicians may become overly reliant on CDSS recommendations, potentially missing nuances that the system doesn’t capture. It’s crucial to determine the most beneficial steps in the diagnostic process where CDSS can truly enhance clinical reasoning without undermining the clinician’s own judgment.
Additionally, EHR-integrated tools that provide time-oriented presentations of clinical data, such as tracking changes in lab values over time, can help support clinical reasoning by offering a clearer picture of the patient’s condition. However, issues like alert fatigue – where clinicians become desensitized to frequent safety alerts – can diminish the effectiveness of these systems, emphasizing the need for thoughtful integration and use of CDSS within EHR systems to optimize clinical decision-making.
5. Telehealth
How do we define it?
Telehealth refers to the use of digital communication technologies to provide healthcare services remotely. It includes a variety of formats, such as real-time virtual visits (synchronous telemedicine), where patients interact with healthcare providers through video or audio calls for diagnosis and treatment. It also covers asynchronous telemedicine, where medical information is transmitted between healthcare providers or between patients and providers at different times. Other forms include telemonitoring, which involves remotely tracking patient health data, and telerehabilitation, where rehabilitation services are delivered to patients in remote locations. Telehealth technologies enable the delivery of healthcare across distances, enhancing access, especially for individuals in remote or underserved areas.
How is it relevant to clinical reasoning?
The use of telehealth in clinical reasoning presents both opportunities and challenges. In synchronous telemedicine, healthcare providers must adapt their clinical reasoning processes to virtual interactions, relying on limited physical examination tools and data gathered remotely. This can impact the accuracy of diagnosis and treatment, raising concerns about potential biases or errors, particularly when person-centered care is the focus. Additionally, shared decision-making may be more complex in virtual settings, requiring extra care in communication to ensure patient understanding and involvement in their own care.
Asynchronous telemedicine, where patient information is transmitted between providers or patients and healthcare systems at different times, also requires adjustments in clinical reasoning. Providers must synthesize information from various sources, such as telemonitoring data or patient reports, while accounting for the risks of delayed or incomplete information, which can impact decision-making.
Smart home technologies, such as those used in ambient assisted living, introduce another layer of clinical reasoning, particularly for elderly or frail individuals. Clinicians need to consider whether a patient’s digital literacy and manual dexterity are sufficient for using certain devices, ensuring that recommended tools provide safety and support without overwhelming the patient. These decisions must balance the potential benefits of independent living with the risks of technology-related errors or patient non-compliance, further influencing the clinical reasoning process.
The D-CREDO Digital Health Tools Virtual Patient
The D-CREDO project plans to explore the design of a novel type of virtual patient, termed the ‘digital health tools VP’. These virtual patients will present interactive clinical scenarios that encourage students to utilize digital tools for clinical reasoning in various contexts.